Stomatitis is an inflammation of the oral mucosa, accompanied by pain, burning, redness, and ulcers. It can occur in both children and adults and may significantly make eating, swallowing, and sometimes even speaking difficult.
What causes stomatitis?
Stomatitis can develop due to various reasons. In many cases, the main causes include bacterial or viral infections, mechanical injuries, vitamin deficiencies, allergic reactions, and other factors.
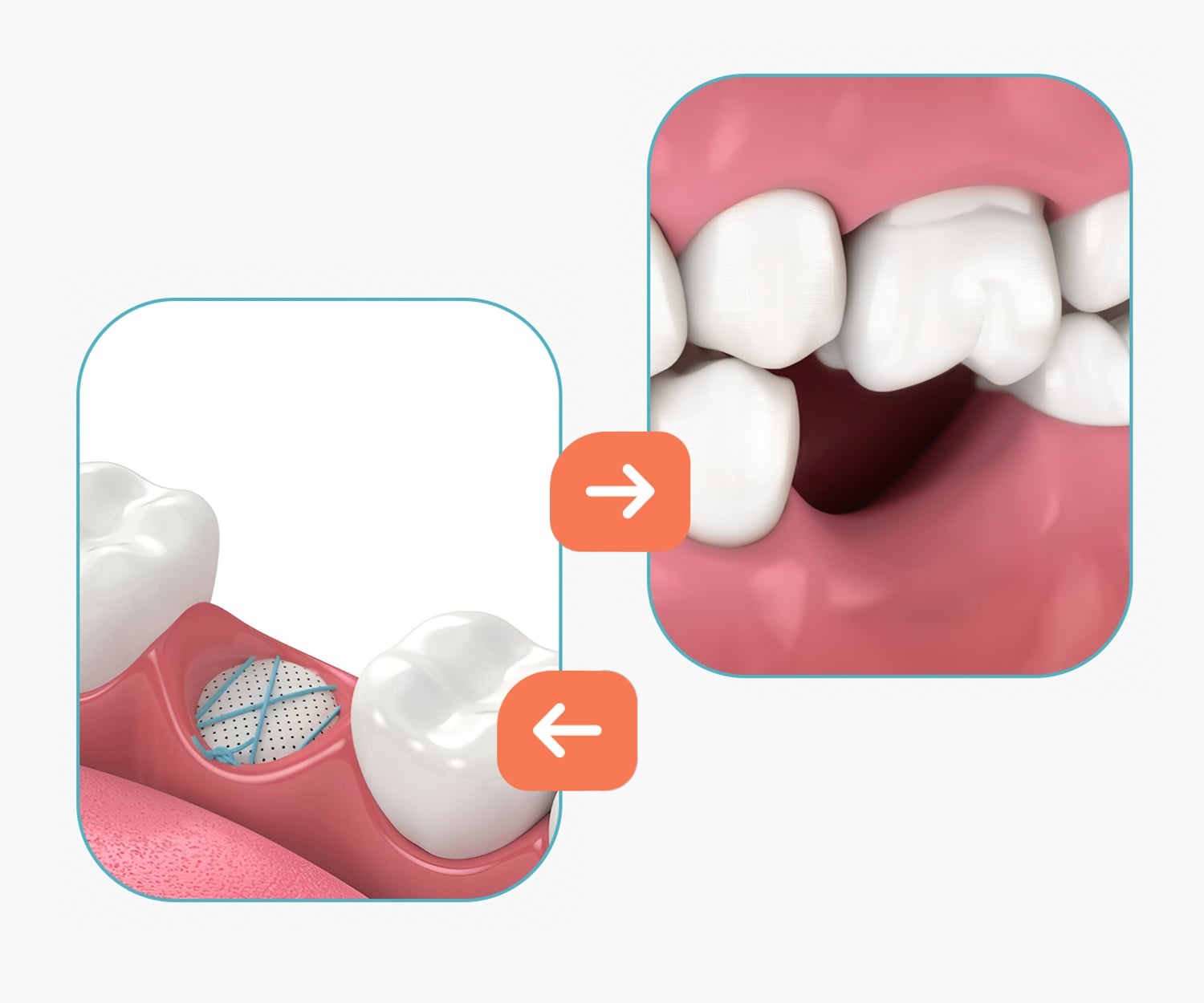
Mechanical injuries – when the oral mucosa is damaged and bacteria penetrate it, for example: accidentally biting the inside of the cheek or lip, a loose crown, a brace wire that irritates the cheek, a newly fitted denture, or trauma caused by a toothbrush.
General health condition – weakened immunity; deficiencies of minerals and vitamins (B12, B1, B6); gastrointestinal problems, which often affect the condition of the oral mucosa; fatigue, stress, and nervous tension.
Hygiene and chemical factors – some toothpastes contain sodium lauryl sulfate (SLS), which can dry out the oral mucosa and contribute to the development of ulcers.
Types of stomatitis
There are many common types of stomatitis. For proper treatment, identifying the underlying cause is crucial, as it helps determine exactly which form of the condition is present.
- Aphthous stomatitis is the most common form, characterized by small, painful ulcers in the mouth. These ulcers are usually white or yellow and are surrounded by a red area. The exact cause of their appearance is often unknown, but it may be related to immune system issues, stress, or vitamin deficiencies.
- Herpetic stomatitis is caused by the herpes simplex virus and is characterized by painful blisters that later burst, forming ulcers. This type of stomatitis is often seen in children and may be accompanied by fever and swollen lymph nodes.
- Candidal stomatitis, or oral thrush, is caused by the fungus Candida albicans. It is characterized by white, milky deposits on the oral mucosa, which leave a red, sometimes bleeding surface when removed.
- Bacterial stomatitis can develop due to poor oral hygiene, a weakened immune system, or a bacterial infection. It often presents with red, swollen mucosa and may be accompanied by pus discharge.
- Allergic stomatitis occurs as a result of an allergic reaction to food, toothpaste, mouthwash, or other substances. It may cause redness, swelling, and itching of the oral mucosa.
Symptoms of stomatitis
- Pain in the mouth
- Ulcers or blisters in the mouth
- Redness and swelling
- Discomfort while eating and speaking
- Systemic symptoms (in severe cases
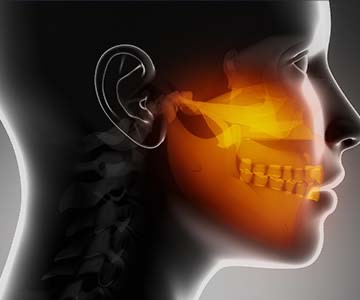
Pain in the mouth is one of the most common symptoms of stomatitis. In some cases, the pain may extend to the tooth nerve, further worsening the patient’s condition.
Ulcers or blisters in the mouth are another significant symptom. They usually appear on the inner cheeks, tongue, gums, palate, or lips. These ulcers can be small or large, single or multiple, and are often surrounded by a red area.
Redness and swelling of the oral mucosa indicate an inflammatory process and are present in almost all types of stomatitis.
Discomfort while eating, speaking, or swallowing is another common complaint. During stomatitis, the oral mucosa becomes more sensitive, making it difficult to consume food, which can lead to nutritional deficiencies, especially if the condition persists for a long time.
Systemic symptoms such as fever, weakness, loss of appetite, and swollen lymph nodes may also occur. These symptoms are more common in viral stomatitis, for example, in herpetic stomatitis.
Symptoms appear in various parts of the mouth: gums, palate, cheeks, tongue, and the lip border.
Treatment of stomatitis
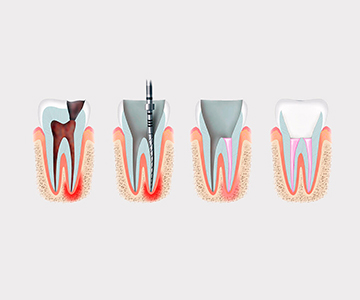
The treatment of stomatitis is a complex process aimed at relieving symptoms, controlling infection, and restoring oral health. The success of treatment depends on proper medical intervention, as well as home care procedures and preventive measures.
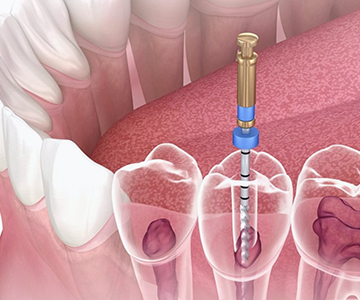
Medical treatment of stomatitis begins with an accurate diagnosis of its type. The doctor primarily prescribes local treatment, which includes antiseptic rinses and pain-relieving medications. In severe cases, systemic treatment may also be prescribed.
Home treatment of stomatitis
Adjusting the diet is an important part of home treatment. During stomatitis, it is recommended to consume soft, non-irritating foods and drink plenty of fluids. Spicy, acidic, and salty foods should be avoided, as they can increase pain and slow down the healing process.
When to see a dentist?
-
If the symptoms of stomatitis do not improve within 1–2 weeks or worsen despite treatment.
-
If the pain is severe and interferes with eating or drinking.
-
If accompanied by a high fever (above 38°C), which may indicate an infection and requires immediate medical attention. Other concerning signs include significantly swollen lymph nodes and rapidly growing or unusually large ulcers in the mouth.
Prevention of stomatitis
Prevention of stomatitis begins with oral hygiene. It is recommended to brush teeth at least twice a day with a soft toothbrush and use mouth rinses regularly. However, studies show that hygiene alone is not enough—maintaining a healthy lifestyle is also important.
Managing stress, eating a balanced diet, and getting enough sleep significantly reduce the risk of developing stomatitis. Special attention should be given to strengthening the immune system through regular physical activity and consuming foods rich in vitamins.
Stomatitis in children
The first signs of stomatitis in children may include irritability and loss of appetite. Later, ulcers appear in the mouth, often accompanied by:
-
Elevated temperature
-
Refusal to eat due to pain
-
Increased salivation
-
Disturbed sleep
Treatment should be prescribed only by a pediatrician or dentist and depends on the type and severity of stomatitis. Typically, treatment includes the use of antiseptics, pain relief, and immune support, while special medications may be prescribed if necessary. Self-treatment is not recommended, as improper care can worsen the condition.
Prevention of stomatitis in children depends on proper oral hygiene, using age-appropriate oral care products, maintaining cleanliness of toys and hands, and a healthy, vitamin-rich diet. Regular preventive visits to the dentist significantly reduce the risk of developing stomatitis and help maintain the child’s oral health.
At Blits Dental - Kakhaber Kharebava Clinic, qualified dentists offer professional diagnostics and modern methods for treating stomatitis. Early diagnosis and appropriate treatment significantly reduce the risk of complications and speed up the recovery process.
To schedule a consultation, contact us at (+995) 32 222 15 16 or book online.
















.jpeg)